Meal Planning is a powerful tool for bettering your health. By intentionally planning foods to eat, you can significantly reduce your risk of another stroke.
Eating a heart-healthy diet after stroke
A heart-healthy diet is recommended for most adults as a way of life and also for people who have had a stroke. What makes up a heart-healthy diet? When you prepare your food, you can create sections on your plate as a guide to help you build a heart-healthy meal.

Lean Protein
Try to eat mostly lean proteins, including chicken, turkey, pork, fish, nuts, grains, and legumes provide healthy options for protein. Proteins to avoid include meats such as steaks, hamburgers, and other proteins that are high in saturated fat.
Whole Grains
Whole grains, like oats, quinoa, brown rice, and whole grain pasta, are high in fiber, which helps manage blood pressure, improve cholesterol levels, and reduce the risk of heart disease. Aim to choose whole grains over refined grains.

Fruits and Vegetables
Rich in vitamins, minerals, antioxidants, and dietary fiber, fruits and vegetables help reduce blood pressure, cholesterol levels, and inflammation. Any fruit or vegetable is a great addition to your diet. When it comes to produce, the motto is “the more the merrier”.
Low-Fat Dairy
Low-fat or fat-free dairy products, like cottage cheese, milk, yogurt, etc. can be a healthy addition to your diet. Be sure to choose low-fat varieties.
Foods to Limit or Avoid
Eating for stroke recovery is also about limiting or avoiding certain foods. Here’s a breakdown of the types of foods to eat less of when prioritizing heart health.
Saturated Fats
Fatty cuts of meat, full-fat dairy products, butter, lard, palm oil, and partially hydrogenated oils found in many fried foods have high amounts of these unhealthy fats. These should be eaten sparingly. It’s okay if you have them occasionally, but keep it to a minimum.
Added Sugar
Sugar-sweetened beverages, candy, baked goods, desserts, and many processed foods like ketchup, flavored yogurts, salad dressings, peanut butter, granola bars, etc. contain an abundance of added sugar. It can be challenging, but aim to limit the added sugars in your food and drinks.
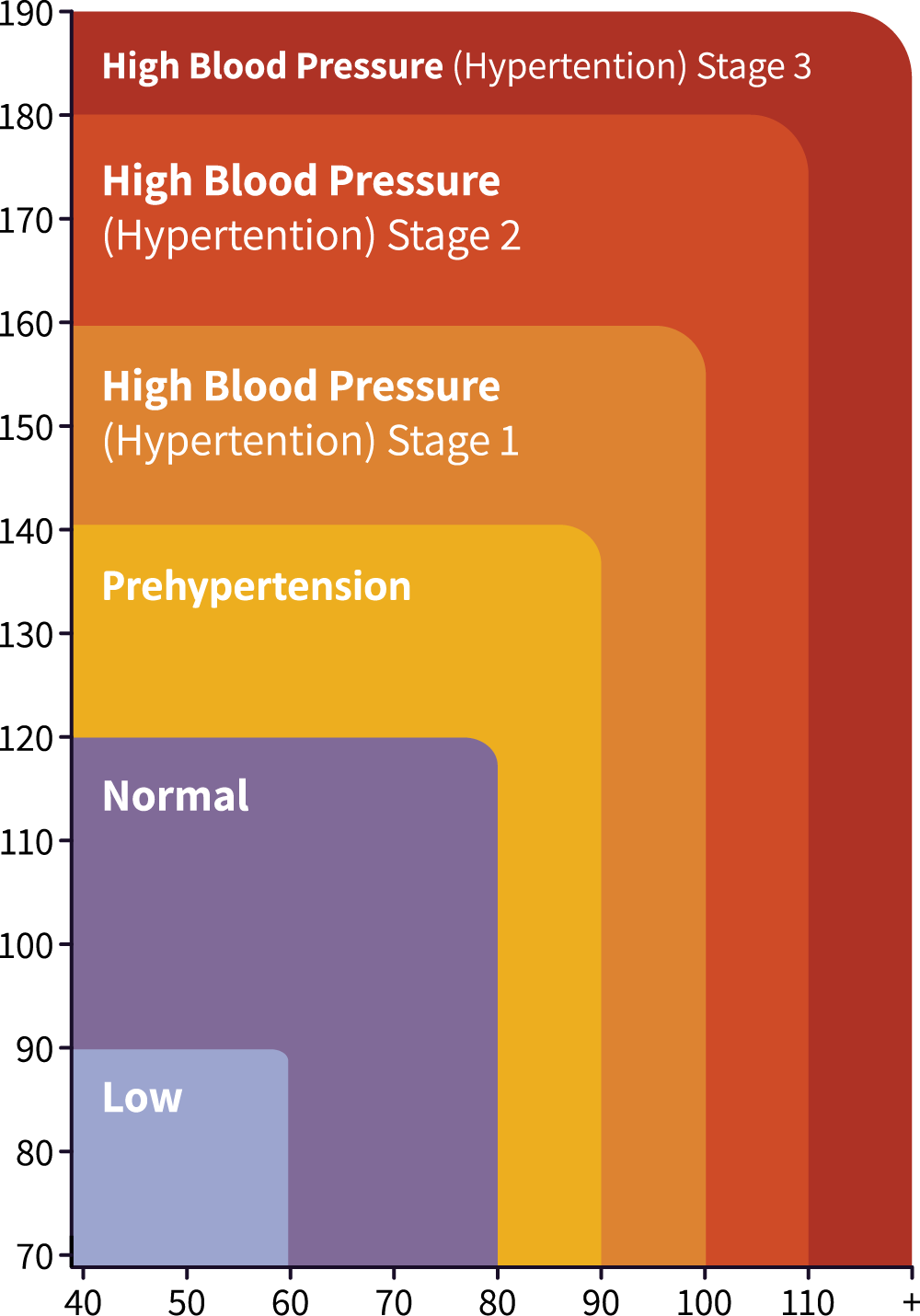
Sodium
Excessive sodium intake can lead to high blood pressure, a major risk factor for heart disease and stroke. There are many hidden sources of sodium including processed snack foods, canned soups, fast food, salted snacks, and even condiments.
Food preparation
Preparing and eating meals can be challenging with limited arm or hand mobility or fatigue. Instead of resorting to processed take-out meals, which lack nutrition, plan your weekly meals. This can help to reduce daily cooking stress and simplify your workload. Write out what you plan to make each day of the week, and shop for foods that help reduce the burden of cooking prep. Experiment with bagged salad kits, pre-chopped vegetables, marinated meats, or even fully-prepared refrigerated meals. These options are incredible resources. Feel free to use them!
To support safe and efficient meal planning, consider the weight and material of the cooking supplies. Here are a list of kitchen tools that may be helpful.
- Easy to open Tupperware for improving accessibility
- Lightweight pots and pans, mixing bowls with handles
- Using appliances like the InstantPot to avoid exposure to a heat flame
- Adaptive equipment to easily open jars and cans
- Dycem to help cutting boards, pots, and bowls from sliding
- Modified cutting boards that address limitations in hand and arm use
Ordering groceries and meals online
Think about utilizing online grocery ordering services or meal delivery services. By carefully reviewing ingredients you can make informed decisions about your purchases. Online ordering also minimizes the chance of impulse buying unhealthy snacks.
Several companies offer complete meal delivery services or provide ingredients along with detailed cooking instructions for preparing meals at home. These meal delivery services often provide fresh, nutritious food options. And the best part? You don’t ever have to leave the comfort of your own home.
Managing food textures
If you experience difficulty swallowing, eating can be challenging. Finding ways to ensure your intake of essential nutrients does not slip is crucial. Creating thick soups can be an effective solution, as they are easy to swallow and can be conveniently stored in the freezer. Keep in mind, it’s best to make soups from scratch as opposed to canned soups in order to control salt and sugar levels.
As always, consulting with your dietitian, speech therapist, or occupational therapist is the best way to get personalized advice based on your individual circumstances. They can evaluate your dietary and eating requirements and develop a plan tailored just for you.
Get support with meal planning.
Kandu Navigators and Dietitians work directly with stroke survivors to support healthy lifestyle and behavior changes that can reduce a survivor’s stroke risk. Our experienced doctors, nurses, and navigators take the time to understand your individual needs, developing personalized recovery plans and providing essential resources to help make recovery a lot smoother.